Posts for Clinical Care Concerns
Missives from Ms Peg Lateral (MJ Fehrenbach, RDH, MS)
or Counsels from Ms Carabelli (J Young-Scholes, (ret.) RDH, ASc)

November 1, 2022
Patient Care Concerns from Ms Peg Lateral
Considerations maintaining our scientific viewpoint.
Saw this posted recently when taking a friend to her weekly hospital visit; one may want to consider its use in clinical areas since a having oral cancer, periodontal disease, endodontics, and caries can be overwhelming for patients... not to mention other health concerns they may have a history with. It helps remind us all!!!
These considerations bring up other related topics that always need a special consideration; see associated CURRENT links to check out below:
BEST HANDOFF TIPS for dental setting (RDH MAG)
ABUSE AND NEGLECT (NIH) REDUCE STRESS (ADA)
PATIENT COMMUNICATION TOOLS (RDH MAG)
MANAGEMENT OF DENTAL PATIENTS WITH SPECIAL NEEDS (AAPD)
LINK BETWEEN DENTAL AND MENTAL HEALTH (CLEVELAND CLINIC)
November 21, 2022
Computer Aided Diagnosis from Ms Peg Lateral
We are zooming in on CAD and how it is aiding in diagnosing periodontitis over time!
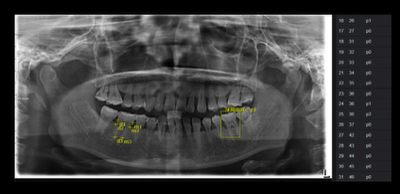
Can you imagine sitting in your dental chair and the computer nearby is aiding you in the diagnosis of the patient's periodontal case using latest classification system? Well, welcome to the future. The figure here has been taken from the research article below (#3). Until then, check out Automated staging and grading app for periodontal records!
From recent study noted below:
"Computer-aided diagnosis (CAD) has been used to identify cavities and periodontitis lesions, as well as maxillary sinusitis, osteoporosis, and other pathologies in the oral and maxillofacial field. It can provide dental professionals with a valuable second opinion by automatically detecting and classifying pathological changes. Recently, CAD based on deep learning have been used extensively for solving complex problems in radiology. However, studies of deep learning applications have been limited in the field of oral and maxillofacial imaging. The deep learning method has been applied to: detect landmarks in cephalograms; detect teeth and classification; diagnose cavities; and detect maxillary sinusitis."
These considerations bring up other related topics that always need a special consideration; see associated CURRENT links to check out below:
See Link #3
December 10, 202
Dementia and Oral Health? from Ms Carabelli
Poor oral health is one of the risk factors for dementia!
As an oral health professional, one of our most important roles is to educate the patient that what manifests in the oral cavity can affect one’s overall health and state of being. There are several microorganisms in the oral cavity that are capable of degrading host tissue. Assessment of soft and hard deposits, removal, and appropriate oral health care measures, particular for that patient, are factors that help maintain one’s overall health.
Dementia (including Alzheimer Disease) result from the death of nerve cells and the ability to communicate between these cells then begins to diminish. Genes do play a role, but no specific abnormal gene has not yet to be associated with any type of this condition. However, major risk factors are being studied that may contribute to the onset of this disease. Poor oral health is one risk factor that is now being considered as a catalyst to dementia or Alzheimer Disease. Thus our role as that a Dental Hygienist can be vital to keeping one’s mental health.
Links to several recent studies:
https://www.sciencealert.com/the-cause-of-alzheimers-could-be-coming-from-inside-your-mouth
https://www.medscape.com/viewarticle/980703 (need to register and there is no downside!!!)
March 25, 2023
Integrated Research Biopsies from Ms Peg Lateral
We need more data such as with integrated research autopsies!
As we start the new year, we need to address a topic that is sometimes hard due to certain factors (see discussion next paragraph). But it is always been that autopies and research go hand and hand in medicine. But not as yet in oral medicine, the new specialty assigned by the ADA. There needs to be collection of craniofacial tissue ASAP as part of biobanking. The new technologies that allow for high-resolution, multimodal phenotyping of human samples, using optimized sampling procedures (possibly of whole jaws with teeth) will then allow for unprecedented understanding of common and rare dental, oral, and craniofacial diseases NOW!
It is true that conventional autopsies are becoming less common due to many factors such as cultural or religious objections, high costs for time and limited personnel, and growing opinions about the lack of an autopsy’s usefulness compared with other diagnostic techniques. But even so conventional autopsy is till used for research purposes, sometimes called the “research autopsy,” that has proven useful for understanding cardiovascular diseases, diabetes, cancer biology, chemotherapeutic failures, and viral pandemics such as COVID-19. Interestingly, all these have also major focuses within orofacial regions and infections related to them. This tendency is highlighted in the linked article as the bidirectional relationship of the orofacial region in the context of extraoral diseases.
Link to opinion article: https://jada.ada.org/action/showPdf?pii=S0002-8177%2822%2900731-0 (can download as needed to share!)
June 6, 2023
Update on Tongue Development from Ms Peg Lateral
Current Research Shows Change in the Players for Tongue Development!
As I was researching materials for the latest sixth edition of Illustrated Dental Embryology, Histology, and Anatomy (Elsevier), I was drawn into a world of new structures along with those that we know that are felt to be involved in tongue development. See below for the draft for that new edition and await the new figures as they are created by the development team!
Body of Tongue Formation
During the 4th week of prenatal development within the embryonic period, the tongue begins its development. The tongue development begins as a triangular median swelling, the tuberculum impar (too-ber-kuh-luhm im-pahr) (Fig. 5.8, A-B). The single tuberculum impar is located in the midline and is formed on the mandibular arch, which is considered the first pharyngeal/branchial arch, on the floor of the primitive pharynx within the embryo's conjoined nasal and oral cavities (see Fig. 4.10).
Later, two oval enlargements develop on each side of the tuberculum impar, the lateral lingual swellings (see Fig. 5.8, A-B). It is important to note that these anterior swellings are from the further growth of mesenchyme of the mandibular arch. The paired lateral lingual swellings grow in size and merge with each other. The rate of growth of the lateral lingual swellings is faster than that of the tuberculum impar. Thus the two fused lateral lingual swellings overgrow and encompass the disappearing tuberculum impar to form the anterior two-thirds of the mature tongue, the body of the tongue, which lies within the oral cavity proper.
The median lingual sulcus is a superficial demarcation of the line of fusion of the two lateral lingual swellings as well as of a deeper fibrous structure (see Fig. 2.14). Thus the tuberculum impar itself does not form any recognizable part of the mature tongue. Around the lingual swellings, the cells degenerate forming a lingual sulcus, which frees the body of the tongue from the floor of the mouth, except for the attachment of the midline lingual frenum (see Fig. 2.17).
Base of Tongue Formation
Immediately posterior to these fused anterior swellings, a large midline swelling is developing from the mesenchyme of the second, third, and fourth arches. It has been revealed that this swelling consists of a copula (kop-yuh-luh) from current research. The copula is also associated with second arch and also an adjacent large swelling. This is the hypopharyngeal eminence (hahy-puh-fuh-rin-jee-uhl eh-muh-nuhns) or hypobranchial eminence that is associated with third and fourth arches. Like the lateral lingual swellings with the tuberculum impar, the hypopharyngeal eminence grows at a faster rate than the copula. Thus the hypopharyngeal eminence overgrows and encompasses the disappearing copula to form the posterior one-third of the mature tongue, the base of the tongue. The copula itself does not form any recognizable part of the mature tongue.
Even farther posterior to the copula and then later the hypopharyngeal eminence is the projection of a third median swelling, the epiglottic swelling (ep-i-glot-ik), which develops from the mesenchyme of the posterior parts of the fourth pharyngeal/branchial arches (see Fig. 5.8, B). This swelling marks the development of the most posterior region of the tongue or its root and site of the future epiglottis.
Completion of Tongue Formation
As the tongue develops still further, the posterior swellings of the base of the tongue, the hypopharyngeal eminence, merges with the anterior swellings of the first arch of the body of the tongue during the 8th week of prenatal development (see Fig. 5.8, C). This fusion is superficially demarcated by the sulcus terminalis on the mature dorsal surface of the tongue, which is an inverted V-shaped groove marking the border between the base of the tongue and its body (see Fig. 2.14).
The sulcus terminalis points backward toward the oropharynx at a small pit-like depression, the foramen cecum, which is the beginning of the thyroglossal duct. This duct shows the origin of the thyroid gland and the migration pathway of the thyroid gland into the neck region. The duct forms an open connection between the initial area of thyroid gland development and its final location. This duct later closes off and becomes obliterated before birth unless it undergoes cystic transformation (see Fig. 11.14). However, no similar anatomic landmark is found between the base of the tongue and the epiglottic region after development.
By the end of the 8th week, the tongue has completed the fusion of these swellings. The tongue then contracts and moves anteriorly and inferiorly to avoid becoming an obstacle to the developing palatal shelves. However, the entire tongue is in the oral cavity proper at birth; its base and epiglottic region later descend into the oropharynx by 4 years of age, while the body remains in the oral cavity proper. Thus the tongue moves out of the pharynx into its correct place in the oral cavity proper. The tongue usually doubles in length and wideness between birth and puberty, which is when it reaches its maximum size.
Reviewing the discussion in this part of the chapter explains how the single structure of the tongue is innervated by various cranial nerves. This is because the tongue develops from the first four pairs of pharyngeal/branchial arches, each with its own cranial nerve. Since the oral mucosa of the anterior two-thirds of the tongue is derived from the first arch, its general sensation is supplied by the nerve of that arch, the fifth cranial or trigeminal nerve. In contrast, since the oral mucosa of the posterior one-third of the tongue is derived from the third arch, its general sensation is supplied by the ninth cranial or glossopharyngeal nerve.
Finally, taste sensation to the anterior tongue is by the seventh cranial or facial nerve associated with the second arch, and again by the ninth cranial or glossopharyngeal nerve to the posterior tongue associated with the third arch. Taste sensation within the epiglottis is also supplied by the tenth cranial or vagus nerve associated with fourth arch.
In contrast to the swellings of the tongue originating from the arches, the intrinsic muscles of the tongue originate from the surrounding mesoderm of the occipital somites and not from the pharyngeal/branchial arches (see Fig. 3.13). Primitive muscle cells from these somites migrate into the developing tongue, taking their motor nerve supply from the hypoglossal nerve or twelfth cranial nerve. See Chapter 4 for further discussion of the development of the innervation of the mucosa of the oral cavity, pharynx, and larynx.
The lingual papillae, smaller elevated structures of specialized mucosa on the dorsal surface, appear toward the end of the 8th week (see Figs. 2.14 and 9.18 to 9.21). The circumvallate and foliate lingual papillae appear first, close to the terminal branches of the glossopharyngeal nerve or ninth cranial nerve. The fungiform lingual papillae appear later, near the terminations of the chorda tympani branches of the facial nerve or seventh cranial nerve. Finally, the filiform lingual papillae develop during the early fetal period around the 10th to 11th weeks.
The taste buds involved in taste sensation and that are associated with certain lingual papillae (circumvallate, foliate, and fungiform) develop during the 11th to 13th weeks (see Figs. 9.16 and 9.17). This is by inductive interaction between the epithelial cells of the tongue and invading nerve cells from the chorda tympani of the facial nerve or seventh cranial nerve as well as the glossopharyngeal nerve or ninth cranial nerve.
October 9, 2023
Update on Arches... from Ms Peg Lateral
Current Research Shows Change Wanted in Name!
There is a consideration to renumber the branchial/phargyneal arches as well as have a renumbering of associated pharyngeal pouches. As you know there is a push from the medical community to the dental community to rename the arches as pharyngeal arches alone since our necks do not have gills. However, this renumbering is a different situation.
This comes from the fact that fifth arch is usually not present. However, many other vertebrates have this fifth arch, and the numbering takes is cue from comparative anatomy. Thus there would be a move to only having arches one through 5 if this change takes hold but only four pharyngeal pouches.
The idea that there are five pouches, as well as six arches has been around for a long time and, for example, can be found in the 1918 edition of Gray's Anatomy (Lewis, 1918). One reason has been suggested that a fifth pharyngeal pouch/ arch forms during development, but this is only transient and regresses later as the embryo matures to the fetus. This concept has not proven by research. The other reason is that this numbering reflects evolutionary considerations.
But a more modern outlook will allow a more complete understanding of the anatomy of the area. Importantly, our embryologic study of the pharyngeal arches has advanced greatly over the last two decades and, perhaps, the most significant development has been the understanding about the formation of the pharyngeal pouches as well as the arches that is key to this needed change.
Branchial/pharyngeal arch development is initiated with outpocketing of the pharyngeal endoderm at points along the anteroposterior axis to form the pharyngeal pouches. These structures then grow to contact the overlying ectoderm, which invaginates to meet them, generating the pharyngeal clefts. It is the apposition between the pouches and clefts that define the limits of the arches, and neural crest cells and mesoderm subsequently migrate into these preformed units. So keep checking on this conundrum and see what happens!
Link to opinion article: A reappraisal and revision of numbering of pharyngeal arches. Journal of Anatomy. 2019.
April 13, 2024
Color Change Issues and Lesions... from Ms Peg Lateral
Updated Diversity with Clinical Lesion Appearance and Darker Skin Tones!
A lesion indicates this change in structure of an organ or part, which can be attributable to injury, pathologic condition, or developmental disturbance. Lesions are common within the head and neck as well as the oral cavity of the adult population. An estimated 10% of dental patients have a lesion. Most of these lesions fall into the category of an atypical finding, a discovery that some clinicians call a variation from normal. However, the lesion could instead be an abnormal finding, a discovery that is not only not typical but is serious pathologic condition, and possibly can even prove fatal, such as with cancer.
Abnormal color changes in the tissue may signal an abnormal finding. Common lesion colors are redder, as in having erythema, or darker red in those with darker skin tones, as well as whiter, with white lesions predominating overall. Other, less common colors include blue, purple, yellow, black, and gray. However, lesions can also exhibit the same color as the surrounding tissue, differing only in other notable ways. Redder or darker red lesions may be the result of increased vascularity in the subepithelial tissue, thinning of the superficial epithelium, or a dissolution of connective tissue. White lesions that cannot be removed with a gauze may be the result of opacity in similar tissue layers from decreased vascularity, excess keratin, or fibrosis, with its increased fibers.
A less common type and possibly fatal form of skin cancer is melanoma, especially if the initial lesion is detected at an advanced stage. In the affected area, multiple colors are present within the lesion, with streaks of tan, brown, or black, and sometimes white, blue, and red, always darker in those with darker skin tones.
Brown, blue, or black lesions indicate a tissue deposit of melanin, blood, or even heavy metal such as amalgam particles with an amalgam tattoo. In addition, fluid-filled lesions or lesions with increased or enlarged blood vessels can appear bluish to translucent, depending on the skin tone beneath. Importantly, all localized brown, blue, or black lesions should be immediately discussed with the patient's dentist, who will quickly refer them to a dental or medical specialist because of the high risk of being metastatic cancer such as with oral malignant melanoma (OMM).
Usually, NMSCs start as small pearly or pale papules on the skin with basal cell carcinoma (BCCs); other forms are redder or darker red in those with darker skin tones such as appearing as a scaly, flat patch or plaque on the skin with squamous cell carcinomas (SCCs).
Approximately 85% of skin cancers are located on the skin of the head and neck because of excessive ultraviolet (UV) exposure from sunlight. Sunlight generates DNA damage that leads to mutation formation and also reduces the host immune system's ability to recognize and remove malignant cells. Most nonmelanoma skin cancer (NMSCs) are from cumulative UV exposure; specifically, melanoma is highly correlated to adolescent exposure. All patients, even those with darker skin tones with lower skin cancer rates, should be encouraged by the dental hygienist to use sunscreen or sun coverage. However, when skin cancer develops in skin with darker tones, it can occur in areas not exposed to sunlight and color changes are not reliable, so it is often in a late stage when diagnosed.
Oral squamous cell carcinoma (OSCC) makes up around 90% of OC/ OPCs and develops from the mucosal epithelium in the oral cavity, oropharynx and larynx. One type of OSCC is verrucous carcinoma (VC), which is a rare, nonmetastasizing, well-differentiated variant. The remainder of OC/OPCs include salivary gland neoplasms, lymphoma, and sarcoma. Importantly, OSCC has a higher mortality rate compared with other carcinomas. The risk of cancerous transformation in ulcerous, redder, or darker red areas in those with darker skin tones is higher than in more commonly found white patches, although the latter can often prove to be cancerous.
From: Fehrenbach MJ. Assessment of Head and Neck Examination. In: Pieren JA and Gadbury-Amyot, C, eds. Dental Hygiene Theory and Practice. ed. 6, Elsevier, 2025.
